Do's and Don't of Motivational Interviewing
Do:
Dig deep: A lot of issues patients experience with food are not about food at all. It’s important to dig a little deeper into our understanding of the patient’s experience to know what may be influencing their behaviors and habits around food.
When you get the feeling that there may be more to the story than these one-liners a helpful way to dig deeper is by doing the following:
Reflect what the patient is saying.
Use Open-ended questions to gather more understanding.
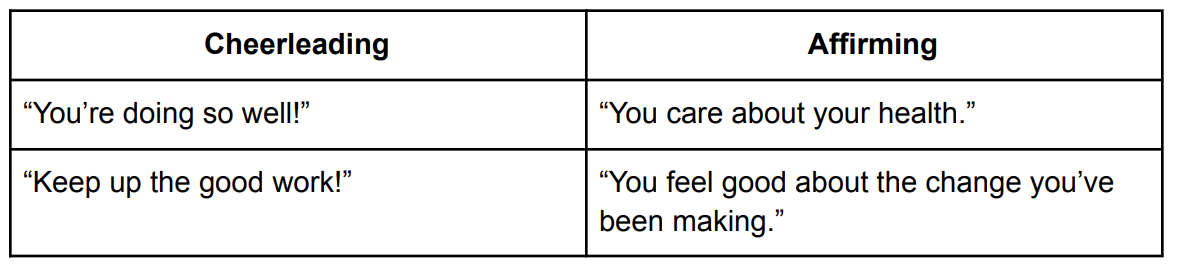
Be affirming rather than cheerleading: Often clinician’s have good intentions when they cheer on their patients. What we want to be careful to avoid though is implying to the patient that they are only successful when they make a change or make them feel like they could disappoint us. A patient may be less likely to share when they are struggling if under this impression. Rather than cheerleading, we can be affirming to help patient’s build self efficacy and confidence in their ability to change.
Ask permission before providing information: In motivational interviewing when we open a discussion, share information, or ask the patient questions, it’s respectful to ask permission first. This invites the patient to be an active participant in the session and encourages autonomy.
Example:
“You had mentioned you were struggling with feeling guilty after eating at restaurants, do you mind if we discuss that further?”
Identify and address possible barriers: In order to help our patients create sustainable change, we need to address any obstacles and barriers that are in between them and their goals. Here are some examples of questions we can ask patients to help identify barriers. We ask to identify barriers ahead of time and retrospectively.
Example:
“How do you feel about the goals set today? Can you anticipate any barriers?”
Normalize ambivalence: Many of our patients will come to sessions feeling ambivalence towards change. Patient’s that are aware of this ambivalence can feel like something is “wrong” with them because they have mixed feelings or lack motivation around change. Something we can do to help our patients feeling this way is to reassure them that feelings of uncertainty and reservations are normal.
Example:
“It makes sense to be a little scared about making this change, you’ve never done this before.”
Hold space for emotions: When working with patients on behavior change, it is really normal for emotions to arise during sessions. As we know, patient’s challenges with food are rarely just about food. Holding space is not a process of helping, healing, or assisting someone directly, but rather being a witness to someone’s emotions without judgment, opinion, or distraction.
Ways to for holding space for patient’s emotions:
Pause and Breathe - Sometimes a patient’s emotions can stir emotions within the clinician or cause a reaction. When a patient has an emotional reaction, take a moment to pause and take a deep breath. Our ability to stay calm will let the patient know that it is a safe place for them.
Listen - Take time to listen instead of asking questions or educating. Avoid thinking about where to go next in the session and just stay present with the patient.
Validate - After listening to the patient, validate their feelings. Remind the patient that their feelings are valid and deserve space.
Don’t try to change or fix it - Sometimes it can feel like a session doesn’t go well if a patient has an emotional response because we didn’t have time to educate or focus on motivational interviewing. Clinicians are not responsible for how the patient shows up but are responsible for their own response to the patient. Sometimes a session that focuses on holding space and active listening can be the most impactful. It also let’s the patient know that they are in a safe space which maintains good rapport and increases the patient’s willingness to share honestly.
Don’t:
Rapid fire question: During an initial assessment or when we are working to gather more information and data from a patient, it’s important we do so without making the session feel like an interrogation. We want to keep sessions personable and conversational. One strategy that can help prevent rapid firing questions is to use a 2:1 ration of Reflections: Open-ended questions.
Use scare tactics: There is an appropriate time and place to discuss the negative consequences of certain behaviors with patients, but focusing on the dangers of behaviors or using inflammatory language that can scare patients has been shown to overwhelm, immobilize, and create feelings of shame for patients.
Pressure, fix, or control: Motivational interviewing can encourage a patient to take the lead in changing their behaviors and managing their health. Clinicians are full of knowledge and ideas and sometimes want to “fix” the patient as a way to control the outcome, unfortunately this often doesn’t work to create meaningful and sustainable change.
Helpful ways to avoid falling into the trap of trying to “fix” or “control” a patient:
Avoid using controlling language such as “you should”, “you must”, “it’s better”, “it’s important”, “do it for me”, “you have to” etc. when counseling.
Avoid arguing or debating the patient. There can be an urge to “right” something wrong a patient says. This also can lead to more defensiveness from the patient and reduce their willingness to be open.
Express empathy. Focus on the patient in front of you as they are and not the outcome you may want for the patient. Assure the patient they are being heard and understood.
Develop discrepancy. Help the patient see the difference between their behaviors and core values. Allow them to find a desire to change for themselves.
Overwhelm a patient with information: One of the pitfalls that can be easy to fall into in nutrition counseling is information overload. It can be easy to want to provide as much education to a patient as possible. If a patient leaves a session with too many tasks or too much information to digest it is less likely they will succeed at the changes they are trying to make.
Here are few ways you can avoid this pitfall:
Slow Down- Remember Rome wasn’t built in a day and behavior change doesn’t happen overnight. In outpatient care our goal is to help patients make sustainable lifestyle changes. It’s important to remind our patient’s and ourselves that we can focus on one topic at a time, and take our time to make sure the patient understands and is able to implement the desired changes.
Pay attention to non-verbal cues from your patient- Notice signs a patient may be overwhelmed or “checked out” in a session. Examples may include developing a glazed stare, seeming distracted, or having an expression of stress or anxiety.
Recognize when we need to take a step back-It’s important that if we recognize, we did overwhelm a patient with information to take a step back and focus on motivational interviewing again instead of education. Education can help plant seeds of change, but motivational interviewing is where the bulk of the growth occurs.
Check in with your patient-Often the best way to know how our patient is to ask them directly. After spending some time on education, it can be helpful to check in with whether our patient feels overwhelmed or not before sharing more or moving on.
“How are you feeling right now?”
“That was a lot of information, how are you feeling about it?”
“Do you want to learn more about XYZ, or do you want to start by focusing on what we just discussed?”
“Let’s take a second to review what I just talked about, what are your thoughts?”
Allow for Steam Rolling: Patient led sessions and collaboration are core characteristics of motivation interviewing as discussed earlier in the training. With that said, it also shouldn’t mean that the RD is passive in session or allowing for patient’s to steam roll.
Here are some strategies to avoid steam rolling in sessions:
Set expectations clearly: Make sure to set expectations for how patient should come to session (no distractions, quiet and private space etc.), what happens in a session (assessment vs follow-up), having regular appointments.
Establish yourself as a nutrition expert: RD’s are not the experts on the patients’ lives or bodies, but they are the experts on nutrition. Establishing this early in patient care can help build patient trust in the information and knowledge shared by the RD.
Re-engage patients if they lose focus: Sometimes patients get off topic or maybe even intentionally avoid certain topics of importance in sessions. A patient led session does not mean that the patient goes completely off focus. If this happens the RD can help the patient re-focus on the topic at hand.
Talk more than you listen: Active listening was discussed earlier in the training, but it cannot be emphasized enough that active listening should be a priority in motivational interviewing. If RD’s are doing the majority of the talking in a session, there is a good chance they are not doing enough motivational interviewing and good rapport is not being built with patients. If the RD is not listening, they can’t reflect the patient. appropriately, they can’t provide relevant affirmations, and they most likely don’t have enough information about the patient to provide effective treatment.