New Chart Note Experience: Overview + How to Get Started
At Nourish, we utilize chart notes to document what occurs in session, record patient updates, and coordinate care with external providers. All charting occurs within your Nourish Provider Portal. To support your workflow, you also have access to the Nourish Scribe, an AI-powered tool that generates a session summary to help you chart more efficiently. The following sections will guide you through accessing, creating, and completing chart notes. Please review carefully so that you feel equipped going into your first session.
Overview
At Nourish, we utilize chart notes to document what occurs in session, record patient updates, and coordinate care with external providers. All charting occurs within your Nourish Provider Portal.
The following sections will guide you through accessing, creating, and completing chart notes. Please review carefully so that you feel equipped going into your first session.
Creating and Accessing Chart Notes
Nourish charting operates entirely within the Nourish Provider Portal. To create and access chart notes:
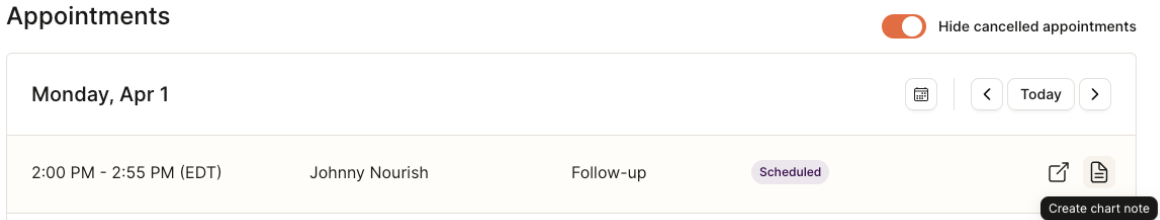
Navigate to the Home page of your Provider Portal, where appointments are sorted by date.
Create a chart note for the desired session by hovering over the chart note icon on the far right of the appointment line item and selecting "Create chart note".
If you have already started a chart note, the same icon will say "Open chart note". Simply click to access.
Once a chart note has been signed and locked, you will see a locked icon preventing further editing.
Chart Note Navigation
The chart note was designed by Nourish's Clinical Product team to maximize charting efficiency, improve clinical quality, and better organize information collected during session.
The chart note follows the Nutrition Care Process to produce comprehensive documentation for clinical care as well as billing and compliance.
All-In-One Chart Note Tab
All fields for documenting a patient session are in the “Chart Note” tab. The “Session Summary” tab leverages AI to generate a quick review of key topics from the session. When you join a Zoom session, AI transcription will be on by default, you don’t need to click anything. See the Loom video for more details. You can end the transcription at any time by clicking the little blue box in the top right corner, and stopping the Zoom app. Check back <2 minutes after your call ends to see the summary. No video is saved - the transcript is just used to generate the AI Summary and auto-fill the chart note where relevant.
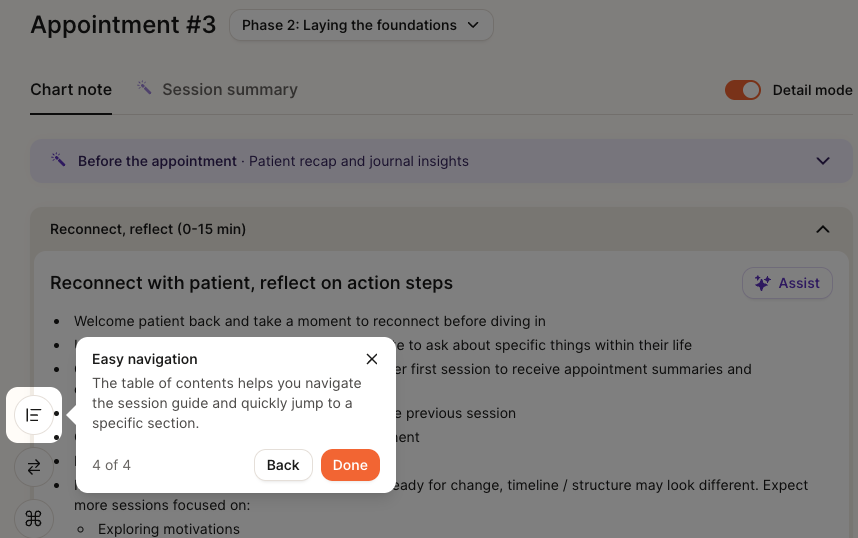
The “Table of Contents” Icon (bottom left of note) provides an overview of each section of the note.
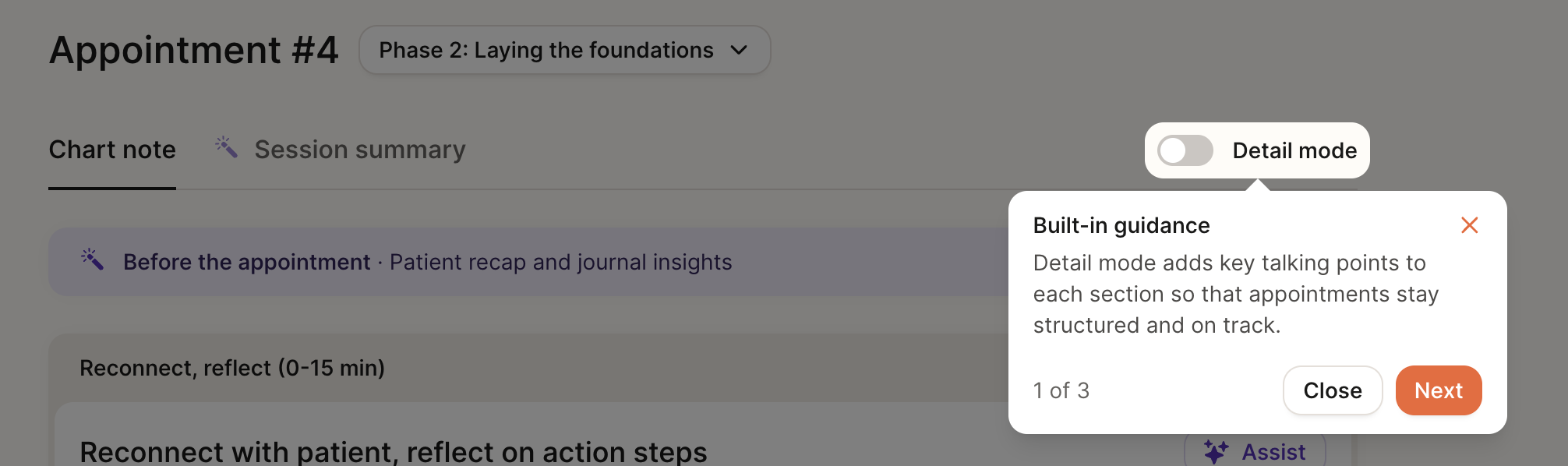
Detail Mode
We offer a “detailed” version of the chart note with additional structure to help guide documentation and support your sessions. When enabled, Detail Mode surfaces additional in-line guidance to help you complete each section of the chart note.
For RDs in their first month at Nourish (based on start date), detail mode is turned on by default.
You can manually toggle detail mode on/off for any chart note. If toggled, your selection will be saved for that session.
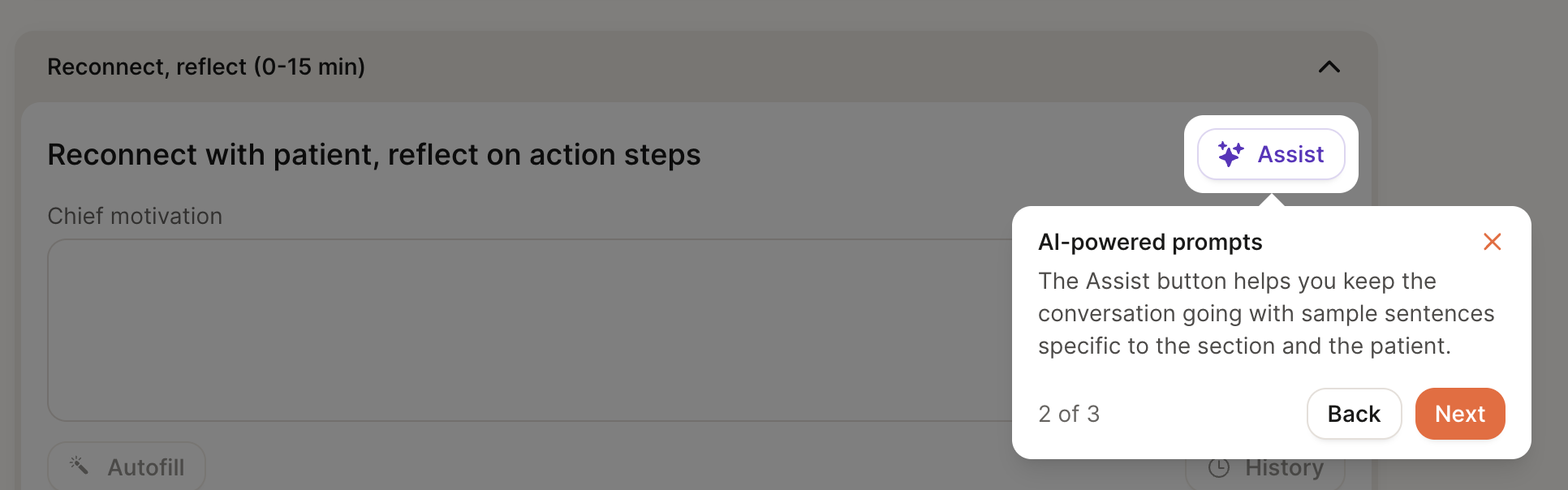
AI Assist
Each section of the chart note includes an “Assist” button, which surfaces example phrases tailored to the patient’s goals, conditions, and previous chart notes. The goal of this feature is to spark ideas for framing recommendations, validating concerns, or guiding the session.
Session Flow
The chart note is organized to follow a suggested session flow, with approximate time blocks to help pace the conversation - for example, an initial flow is structured as:
First 15 minutes: Build connection & set expectations for course of care
15-40 minutes: Assess health history, review intake questions, conduct 24-hour diet recall, and complete PES statement
40-53 minutes: Co-create action plan and wrap up session
These time blocks are meant to inspire structure, not impose rigidity. We encourage you to leverage this framework as a guide - not a script. Every patient is different, and the most effective sessions adapt in real time to what the patient brings into the conversation.
If your patient heads in a different direction, follow their lead, meet them where they’re at, and don’t feel pressured to force a transition just to stay “on track.” The session content will still be there next time, and many topics can easily roll into the next session if needed.
We encourage you to think of this structure as a tool to support your clinical flow - one that helps maintain focus without compromising personalization, flexibility, or patient trust.
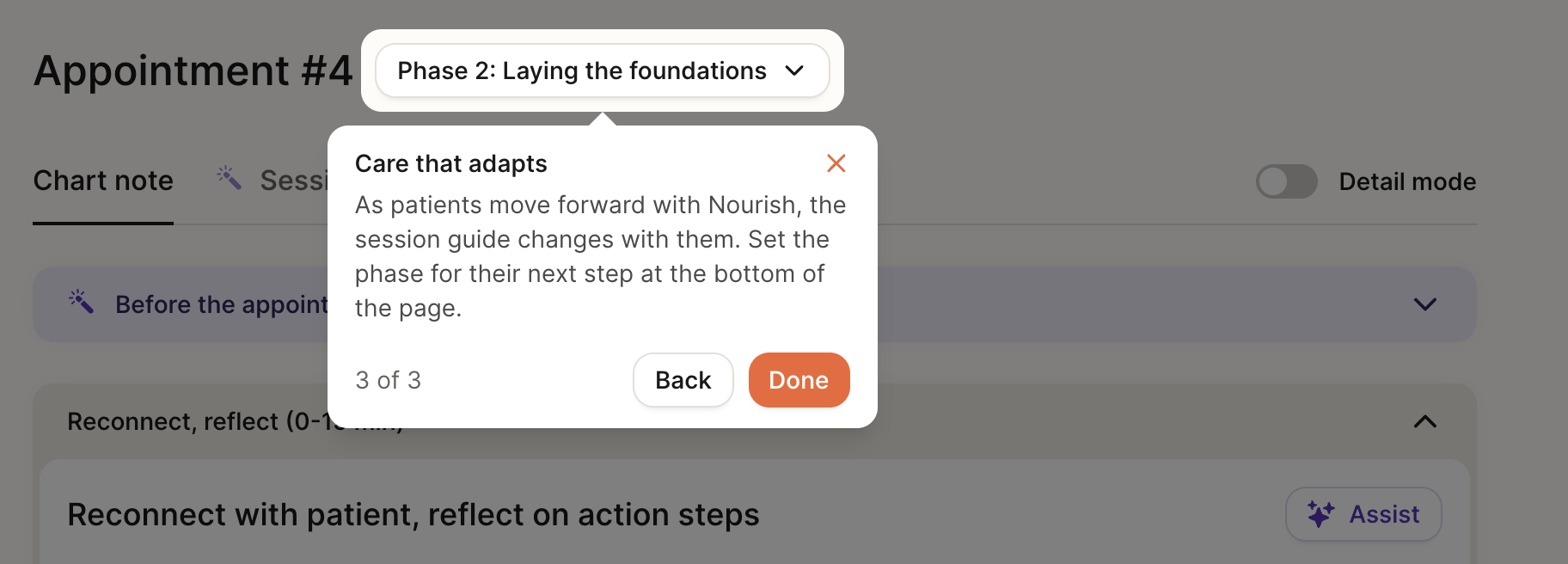
Phase of Care Navigation
Our care model follows a 4-phase care journey, designed to drive measurable outcomes through a blend of behavioral coaching, clinical nutrition care, and personalized goal-setting - all tailored to each individual patient. The Chart Note structure will slightly adjust based on the patient’s current phase of care.
Phase 1: Initial intake
Builds rapport and trust, setting the foundation for a strong, collaborative relationship
Collects medical history, goals, lifestyle habits, and personal goals
Develops a personalized care plan based on the patient’s condition and long-term goals
Patient gets access to the Nourish app for tracking progress: macro tracker, meal photo logging, and device sync (via Apple Health integrations and others)
Phase 2: Laying the foundations & education (typically appointments 2-5)
Weekly sessions to reinforce foundational habits and early behavior change
Focus on education, habit change, and early wins
Ongoing RD engagement through app-based logging, progress tracking, messaging, and asynchronous RD support between live sessions
Phase 3: Building on success (typically appointments 5-8)
Patient progress is evaluated across both clinical outcomes (e.g., A1C, weight, symptom improvement) and behavior change
Care plans are adjusted using trends from food logs, lab / CGM data, and patient-reported outcomes
Patients are supported in interpreting metrics and maintaining momentum
Phase 4: Planning long-term care (typically appointments 8+)
As goals are achieved and outcomes stabilize, care shifts toward long-term habit reinforcement and sustainability
RDs provide education, planning, and structured options for relapse prevention or future re-engagement
Patients may move to lower-frequency check-ins or pause care with confidence, while remaining connected through the app
While Phase 1 is always reserved for the initial session, you have the discretion to move patients from Phase 2 → Phase 3 → Phase 4 based on their progress.
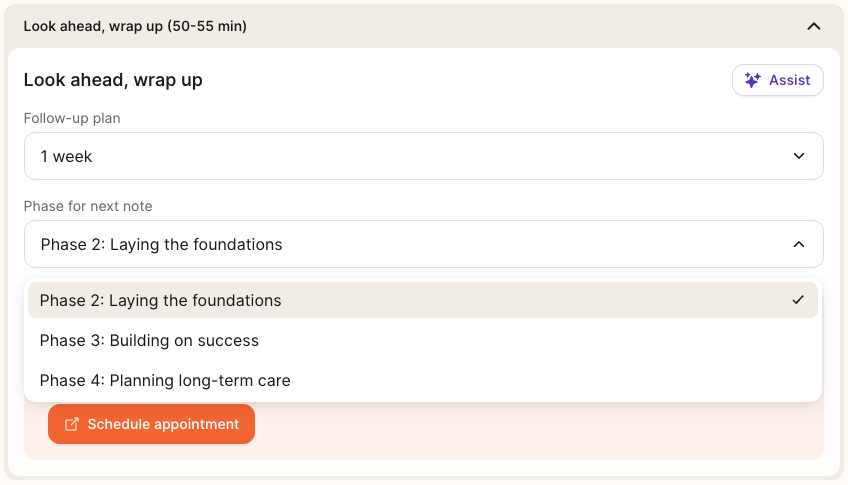
You can transition patients between phases of care using the dropdown at the bottom of the chart note under “Phase for next note” to set yourself up for success in the next session. If you’ve opened a chart note and want to change the phase, there will also be a dropdown at the top of the page.
Below are guidelines to help you evaluate a patient’s readiness to advance. In general, we recommend progressing a patient to the next phase once they’ve met at least one time/session goal and one progress goal.
Phase 2 → Phase 3:
Time: At least 30 days since start of Phase 2
Session: At least 3 completed sessions in Phase 2
Outcomes Data: Completed 1+ patient questionnaire or logged metric (e.g., weight, A1C, symptom check-in)
Goal progress: Patient has made foundational progress towards both short- and long-term goals
Phase 3 → Phase 4:
Time: At least 30 days since start of Phase 3
Session: At least 3 completed sessions in Phase 3
Outcomes Data: Completed 2 or more patient questionnaires or logged metrics (e.g., weight, A1C, symptom check-in)
Goal progress: Patient has made meaningful progress towards both short- and long-term goals
Phase 4 → Maintenance (Stay in Phase 4) or Pause:
Transition to Maintenance Cadence (e.g., monthly, every 2 months) when...
Patient has met most goals but still benefits from accountability
Progress is stable but still improving
Patient prefers continued support at lower frequency
Clinical judgement aligns with ongoing support
Soft Close (care paused, return as needed) when...
Patient has achieved core goals and feels confident continuing independently
No active metrics or behaviors requiring follow-up
Patient is interested in stepping away but wants to know support is available
No clinical concerns
Chart Note AI Summary
At the beginning of both initial and follow-up sessions, the AI Summary feature will compile key patient information within the chart note. When you open a chart note for the first time, the system will begin generating a summary of the patient using their onboarding details or data from previous sessions. This process takes approximately 15-60 seconds, after which you can click “Read More” to view the full summary.
The purpose of this feature is to:
Provide RDs with a concise and actionable overview of patient history, goals, and progress.
Save time in preparing for initial and follow-up sessions, allowing RDs to focus on delivering personalized care.
Strengthen the patient-provider relationship by enabling dietitians to seamlessly pick up conversations and celebrate progress.
If you don’t see this feature, try refreshing your browser using Command-Shift-R (Mac) or Ctrl-Shift-R (Windows).
Chart Note AI Scribe
The Nourish Scribe is an AI-powered tool that generates a session summary from your Zoom recording to support faster, more focused charting. It allows you to stay present with your patient during the session without needing to take detailed notes in real time. Many dietitians report completing their charting in under 5 minutes when using the scribe, and find it helps reduce end-of-day documentation stress. You stay in control of what’s included in the chart — nothing is added automatically, and you can choose which parts of the summary to use.
Click here for the Slack announcement!
Chart Note Structure - Initial Session
Much of the information within the Initial Session chart note will be pre-populated from the patient's intake form. Review and supplement, as needed.
If a patient is transferring their care to Nourish from another platform in which the RD was previously seeing them, a comprehensive nutrition assessment must be documented.
Build connection, set expectations
Chief Motivation: Capture the patient’s core motivation for seeking care - their “why.” This might include personal goals, health concerns, or meaningful life changes they hope to achieve through nutrition support.
Assess, educate, strategize
Conditions: Confirm or update the patient’s primary and secondary conditions. Be sure to check the confirmation box - this is required to sign the note.
Please view the “Managing Patient Conditions in Chart Note” article for additional guidance.Personal & Family Medical History: Review and edit intake form responses as needed. Enclose retained patient-written text in quotation marks.
Focus on relevant clinical history; labs, lifestyle, and meds are addressed later.Height, Weight, and BMI: Record height and weight during the initial session; BMI will be calculated automatically. Update weight as needed and record any relevant weight history and context (e.g., recent changes, history of dieting) if clinically relevant.
Labs & Progress: To add a new lab or test entry, select Add labs or progress and a pop-up modal will appear. To see historical labs & progress questionnaires, select the clock icon next to the header of the section.
Medications: Add medications from a dropdown list gathered from the National Library of Medicine at the National Institute of Health (nlm.nih.gov).
You will need to find the medication by typing in the Name field, then add the relevant Dosage, Frequency, Start date, and End date (if the patient is no longer taking the medication), before selecting Save changes.
After saving, you will be able to edit the end date of the medication by selecting the three dots next to the medication, selecting Edit end date, and changing to the relevant date.
If you need to change frequency or dosage, you should re-add the same medication or supplement again, this time at the different frequency &/or dose.
Lifestyle: Summarize lifestyle factors and intake screen responses that impact care.
Diet Recall: Record a recent diet history for the patient. Import patient meal log data from the Nourish app by selecting Import Logs.
Diagnoses: Nourish documents diagnoses using PES (Problem, Etiology, Signs/Symptoms) statements, a standardized format used in the Nutrition Care Process. Selections are from the 2024 eNCPT (electronic Nutrition Care Process Terminology) standardized language for the PES statement.
To add a new PES, select Add new within the section.
The Problem list is single select and and cannot be edited after the individual PES is saved.
The Etiology list is a dropdown based on your selection for Problem. It can be edited later but will be locked for the current note once signed.
The Signs & Symptoms are multi-select based on a category, and should include additional context in the “More details” field to describe the specific patient situation. These can also be edited in future notes but are locked once the note is signed.
You can mark a diagnosis as resolved (via the three-dot menu), or delete it if no longer relevant, though deletion should be rare. Past PES statements will still be viewable in historical notes.
Ensure inclusion of supporting evidence for your PES statement. For example:
If using “Lab work and tests – abnormal or worsening” as a sign/symptom, include specific lab values in the chart.
If using “Maladaptive eating patterns,” document which behaviors you're referencing.
A PES statement is expected in most chart notes, especially when follow-ups are scheduled or interventions are in progress. However, a PES statement may not be necessary in the following situations. These exceptions should be clearly documented in the chart to ensure accurate and complete records.
The patient's nutrition problems have been resolved, and they are transitioning to a maintenance cadence or pausing Nourish care.
During an initial assessment, no nutrition problems are identified, and no follow-up appointments are planned.
Interventions: Document what you did in-session to resolve the nutrition diagnosis (PES). There are four possible intervention categories, and you can select more than one. After selecting, add details to the intervention(s) as shown below. (See attached pdf at bottom for sample interventions.) Intervention Details should not speak directly to the patient or simply be a list of short term goals, but rather focus on what the Dietitian provided to the patient in session.
Drive retention, create plan
Long-term goals: Long-term goals are internally-facing outcomes to guide care across sessions and should align with the PES and intervention(s). These goals are not visible to the patient. Examples of long term goals include: Improved lab value, Gradual weight loss, or Improved relationship with food or body.
Short-term goals: Short-term goals are patient-facing actions outlining how the patient will apply the nutrition interventions between now and the next follow-up session. Short-term goals can be edited and marked complete by both patients and dietitians. Short-term goals should align with the PES and intervention(s).
Set macro goals (if applicable): Enter appropriate energy needs by calculating macronutrient ranges for your patients.
See the Calculating Energy Needs & Macros for Patients article for additional guidance.
Look ahead, wrap up
Follow-up plan: Best practice is to schedule at least 4 weekly, recurring appointments in the initial session to maintain momentum and reinforce behavior change. Leverage the built-in scheduling tool at the bottom of the chart note.
This will open a new tab to the calendar and will be prefilled to include 4 recurring, weekly sessions from the initial session. In follow ups, if the patient does not have another session booked, the calendar will open to suggest 1 follow up session.Phase for next note: Select the appropriate Phase for your next session with this patient. Please reference the above section on “Phase of Care Navigation” for guidance on when a patient may be ready to move forward in their care journey. Please use your clinical judgment and consider the patient’s unique needs when deciding whether more or less time is needed in the current phase.
Send AI summary, lock note
Appointment Summary: Anything included in the appointment summary box will be e-mailed to the patient once the chart is signed and locked. Use the AI-generated summary as a starting point and personalize as needed. These summaries should speak directly to the patient and include key discussion points and short-term goals covered during the session.
Chart Note Structure - Follow-up Sessions
Reconnect, reflect
Chief Motivation: Record the patient’s main motivations for seeking out care, focusing on their goals and motivations.
Patient Update: Only include what was discussed in this specific session. It does not need to be exhaustive, rather, should be a short summary of key topics.
If there are updates to any of the patient's medical history, lifestyle, labs & tests, or anything else from the Assessment & Diagnosis, they should be made directly in those questions.
Previous patient updates can be viewed by selecting View all. Given the historical storing, do not leave past patient updates within the note.
Diet Recall: Record a recent diet history for the patient. If helpful, view past diet recalls by selecting View all. Select Import Logs to import patient meal log data from the Nourish app.
Revisit baseline / analyze progress
Height, Weight, and BMI: Update weight as needed and weight history as appropriate.
Labs and Progress: Add a new lab or test entry as available and relevant to care. To see historical labs & progress questionnaires, select the clock icon next to the header of the section.
Medications: Add or edit medications as relevant to maintain a full picture of patient condition.
Conditions, Personal & Family Medical History, Lifestyle Assessment: Update as relevant or as new information is gathered.
Educate, build skills, apply
PES statements: Revisit as relevant or as new information is gathered.
Interventions: Document what you did to resolve the nutrition diagnosis (PES). Nutrition interventions should directly address the nutrition diagnosis (PES). Intervention Details should not speak directly to the patient or simply be a list of short term goals, but rather focus on what the Dietitian provided to the patient in session.
Review goals, realign
Revisit and edit Long-term Goals and Macro Goals fields as relevant or as new information is gathered.
Short-term goals: Revise and realign short term goals to patient’s evolving action plan. Short-term goals should outline how the patient will apply the nutrition interventions between now and the next follow-up session. Short-term goals are visible to the patient and can be edited and marked complete by both patients and dietitians. Short-term goals should align with the PES and intervention(s).
Look ahead, wrap up
Follow-up Plan: Indicate when you plan to see the patient next. Best practice is to schedule at least 3-4 appointments booked out to maintain momentum and reinforce behavior change.
Phase for next note: Indicate whether patient should remain within current phase of care, or if patient is ready to move to next phase. Please refer to above guidelines to inform this decision.
Send AI summary, lock note
Appointment Summary: Generate and refine AI summary and email follow-up message.
Signing and Locking Chart Notes
Chart notes must be signed and locked within 48 hours.
Once you have completed your chart note, simply click Sign and Lock. Remember, appointment summary content will automatically be sent to the patient once the chart note is signed and locked, so be sure to review the appointment summary beforehand.
Patient Sidebar
The patient sidebar contains supplemental information you may wish to access easily while in session or while charting. Open the patient sidebar by selecting the icon on the right side of your chart note. Press the same button (relocated to the bottom of the sidebar) to collapse the sidebar.
At the top of the patient side bar, you can see the date of the next scheduled session and easily access message history. Further detail can be opened within the following sections:
Profile: View personal information, contact information, tags, conditions, and sign-up and referral details.
Notepad: A place to record any information not captured within the chart note(s). Use this to keep track of key details about the patient's life, upcoming events, or reminders about what to discuss in future sessions. Notepad content is not shared with the patient nor external providers.
Appointments: View appointment history, upcoming scheduled sessions, and access historical chart notes.
Insurance: View insurance information and past claim statuses.
To-do list: View all active, completed, and deleted to-dos; a more extensive history than what is shown within the chart note.
Outcomes: View all historical outcomes (excluding data from current chart notes), such as lifestyle data, labs & tests, and progress questionnaires.
Scheduling Appointments from the Chart Note
To schedule an appointment directly from your chart note, simply click the Schedule Appointment button in the Wrap-up section of the chart note. This will link to a view of your calendar, and the default date will pre-populate as one week from the date of the chart note appointment, though you're welcome to change that to whatever date you wish.